October 29, 2020
Dear Humans of the Internet,
Let’s get one thing straight right out of the gate: I am not a doctor. I sell advertising. Before that, I worked in retail and at a bar.
What I am is a lifelong fan of medical dramas — ER, House, New Amsterdam, The Resident, Transplant, Code Black and Grey’s Anatomy. Yep, big fan.
I’ve watched enough medical dramas to know how the stories go: a rare diagnosis, a risky or unprecedented procedure, and the miraculous save. Mine had all of that — except it was real, and there were so many plot twists I wouldn’t have believed them if I weren’t the one living them. On television, the music cues tell you what to feel; in real life, there’s only uncertainty and the voice in your head telling you not to panic.
I’ve come to think of it an adrenaline-filled roller coaster. If that’s true, maybe it will make for an interesting read. I’m not trying to squeeze it into a 43-minute episode or cut to commercial breaks, so I’ll just start at the beginning and tell it straight. It’s long. I understand if you don’t make it to the end.
But before I get started, I want you to have this upfront:
When life throws you a crisis, the best way to navigate it is to focus on what you can control.
Feedback welcome,

Act One: The Conflict
The journey started in June 2018, on a Thursday. My husband and I were excited to expand our family. Three children felt like the right number.
We were sitting alone in the exam room, studying the ultrasound photo the tech had left behind and making gender predictions, when the doctor came in. Her tone was careful but deliberate. She was concerned about something called “cesarean scar ectopic pregnancy”.
I recognized the word “ectopic” because ectopic pregnancies were popular plots on primetime medical dramas. But my “TV MD” told me “ectopic” meant a pregnancy in a fallopian tube, which made no sense. I was literally holding a photo of a baby that was clearly inside my uterus. Naturally, I had a lot of follow-up questions.
Here’s what I learned:
- Ectopic actually means “in an abnormal place or position.”
- Ectopic pregnancies occur in about 1-2% of all pregnancies.
- The fallopian tube is the most common place for an ectopic pregnancy to occur.
- A Cesarean Scar Ectopic Pregnancy — or Cesarean Scar Pregnancy (abbreviated CSP) — is rare and potentially fatal. It happens when the placenta implants into the scar from a previous cesarean. As the pregnancy progresses, the placenta can grow through the scar and into other organs, or tear the uterus open, causing catastrophic bleeding.
It was a lot to digest, but at that point, it was just a suspicion and not yet a diagnosis.
To confirm it, I needed a specialized ultrasound from a provider in a different medical network. The first available appointment was four days later. The only thing I did know for certain in that moment was that I was seven weeks and four days pregnant.
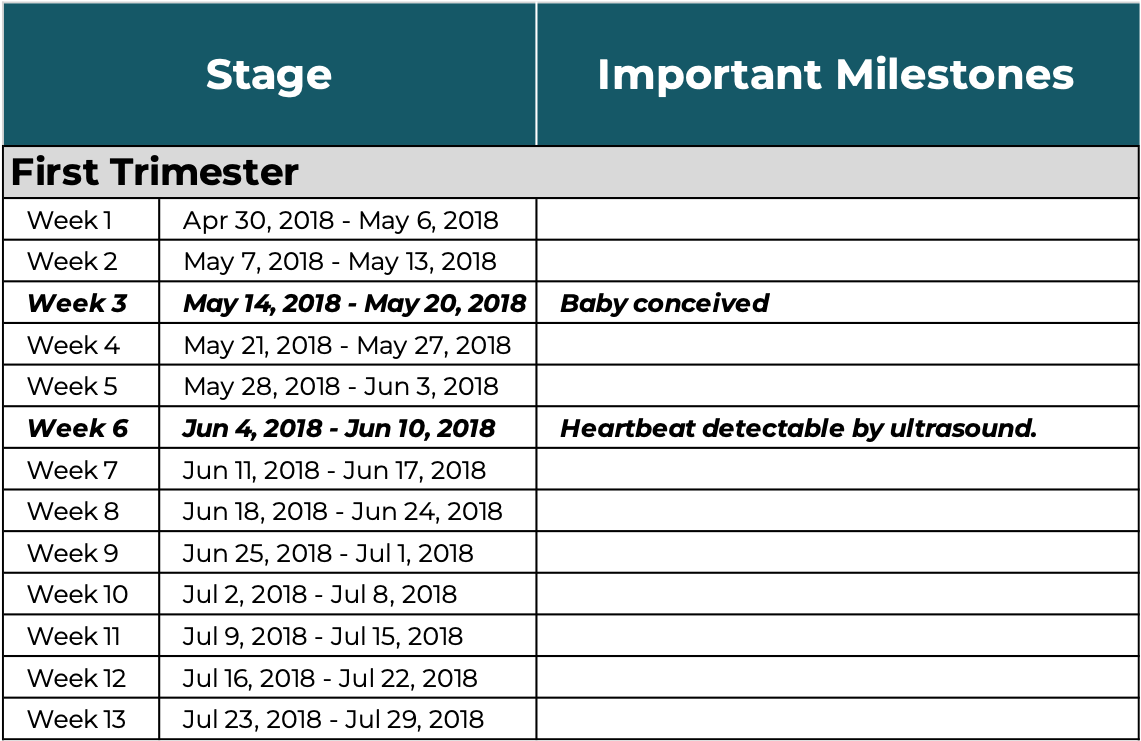
Quick pause for a few pregnancy facts [because I didn’t learn most of this until my first pregnancy].
In Hollywood, a “full-term” pregnancy is usually described with the blanket term, “nine months”. In medicine, it’s a little more precise. Due dates are calculated as 40-weeks from the first day of your last menstrual period [LMP], what’s known as “gestational age”. Doctors use the format XwXd to represent progress; for example, seven weeks and four days becomes 7w4d.
A full term pregnancy is anything after 37 weeks [the start of your 9th month]. The ideal timeframe is 39-41 weeks. Based on my LMP, my estimated due date [EDD] for this baby was February 3, 2019.
This chart shows the full pregnancy timeline using this medical dating formula, with key developmental milestones to illustrate how a cluster of cells becomes a baby.
Pregnancy Calculator by Week
Last Menstral Period: 4/28/2018
To pass the time between appointments, I did what most people do when they’re scared about a pending diagnosis: I turned to Google. The deeper I went, the darker it got.
Most of what I found fell into two categories: clinical case reports and personal accounts from women who had chosen to end their pregnancies because their own lives were at risk. The journal articles were sterile and statistical, describing procedures, drug regimens, and, often, maternal deaths. I did not find a single instance of a cesarean scar ectopic pregnancy that resulted in a healthy delivery.
One story stayed with me: a woman who refused to terminate for religious reasons. Her uterus ruptured at 39 weeks. She suffered a massive hemorrhage and died on the operating table. The baby did not survive either. Somewhere, another child was left without their mother.
My takeaway? Outlook not great…
By the time Monday arrived, I was bracing for the worst. The specialist confirmed what we already suspected: this was dangerous, and I was lucky “we” caught it early. Then she sent me back to my regular doctor to discuss next steps.
I called my husband and left a voicemail. He was on a cross-country flight for work. I imagine it was the worst message he has ever received.
Quick pause to talk about the role of “a support person”.
Support can take many forms — physical, emotional, financial. I’ve had to navigate my share of crises over the years; in my family we jokingly call that “Growing up Herzog“. Jokes aside, those experiences taught met how vital it is to have support when life falls apart.
I had a lot of support through this entire experience. Family and friends showed up for me in ways I’ll never forget. You know who you are, and I hope you know how deeply grateful I was to have you.
But there was one person whose support never wavered: my husband. Even though this was happening to us, he recognized that it was also happening inside of *my* body. I suspect there were moments when he was close to breaking, but he never let me see it. He stayed steady, strong and present — then and now, as I write this heartbreaking story. He is my person, he always supports me. He is also the one who reminds me, over and over, to focus on what I can control. It’s one of the many reasons why I love him.
There were times in this story when he couldn’t be there physically. Every single time, it was because of work. He runs a small business and, like most small business owners, keeps a lean operation. Sometimes he had to choose between being by my side or doing the work that kept our family afloat. Every time we agreed he should prioritize revenue — and every time, ironically, something awful happened. I want to be clear: his absence was never a lack of support. It was just brutally bad timing.
It took me eight minutes to walk from the specialist’s building to my doctor’s office. I managed to pause my sobbing long enough to check in with the receptionist, then was quickly ushered into an exam room — where I resumed crying while I waited.
My regular doctor wasn’t in. Instead, a colleague I’d seen once during my second pregnancy came in and began with the familiar talking points: this was very dangerous, and I was lucky we caught it early. Then she outlined three treatment options. It took only seconds to realize that each one was a different form of termination. I recognized all of them from my four days of obsessive Google research, but this time it felt different. This time, it was real. It was happening to me.
It is probably a good time to let you know that when I am having a hard time understanding something, I find it useful to draw a comparison to something that I do understand. Yes, that is the definition for “analogy” and I recognize that I could have just said, “I make a lot of analogies”. Yet, I felt that it was important to describe the mechanics behind how my brain tries to tackle things that it originally cannot comprehend.
My analogy for this moment is the colorful spinning beach ball icon on a Mac — it indicates processing.
The doctor must have seen that look on my face, because her tone shifted. She said, firmly and clearly, “We cannot allow this pregnancy to continue.” She waited until I met her eyes. “Your life is at risk1.”
It took a minute for the words to register. In my head I was thinking, “Where is Dr. Addison Montgomery-Shepherd? Where was the impossible, never-been-done-before solution that could be pulled off between commercial breaks and end with me holding a healthy baby?”
Once I accepted that the magical TV doctor wasn’t walking through the door, I shifted from speechless to relentless questioning.
I don’t remember everything I asked, only that most answers began with “We don’t have enough data.” Cesarean scar ectopic pregnancies are that rare. For example, when I asked, “If ectopic pregnancies represent 1–2% of all pregnancies, what percentage are cesarean scar ectopics?” there wasn’t enough data to say.
I wasn’t satisfied with the “not enough data” response, so I tried a different approach: “How many patients with cesarean scar ectopic pregnancies do you see a year?”
The doctor paused to calculate and responded that in their practice of about 1,200 patients, they typically see one cesarean scar ectopic pregnancy per year.
ONE! Out of twelve hundred. Which meant I had a 99.92% chance of not having a cesarean scar ectopic pregnancy — and I was the exception.
The questions kept coming. Most of the answers circled back to the same point: if we did nothing, I could die. Then she walked me through the benefits and risks of each treatment option.
A summary (click + to expand):
#1 Do Nothing
Description: Proceed as a high-risk pregnancy.
Benefit: A baby — possibly.
Risk: The odds weren’t in my favor, which was why this option was strongly discouraged. On paper, it could lead to a live birth. In reality, the data suggested it was far more likely the pregnancy would cause uterine rupture and massive hemorrhage — the kind that ends in a transfusion, a hysterectomy, or the deaths of both mother and baby.
#2 Surgery
Description: A range of surgical procedures designed to immediately terminate the pregnancy.
Benefit: Immediate impact.
Risk: The most invasive and highest-risk approach. It carried the same potential for rupture and hemorrhage — and the same possible outcomes: transfusion, hysterectomy, or death.
#3 Medicine
Description: A single or series of methotrexate injections to slow and stop the pregnancy, allowing the body to absorb the tissue naturally, similar to a miscarriage.
Benefit: The least invasive and lowest-risk option; best chance of preserving future fertility.
Risk: The usual chemotherapy-style side effects — nausea, fatigue, stomach pain, mouth sores, hair loss, liver or kidney strain, and increased risk of infection.
#4 Hybrid
Description: A single injection administered directly to the fetus to stop growth, followed within 48 hours by a Dilation and Curettage (D&C) to remove the tissue.
Benefit: A relatively quick resolution.
Risk: Invasive and risky — combining drug side effects with the same potential for rupture, hemorrhage, transfusion, hysterectomy, or death.
My quick assessment was simple: this sucks. It was an awful situation, and I hated that I was the one who had to navigate it. Still, it was happening — and what came next was up to me. The longer I waited to decide, the greater the risk to my own life became.
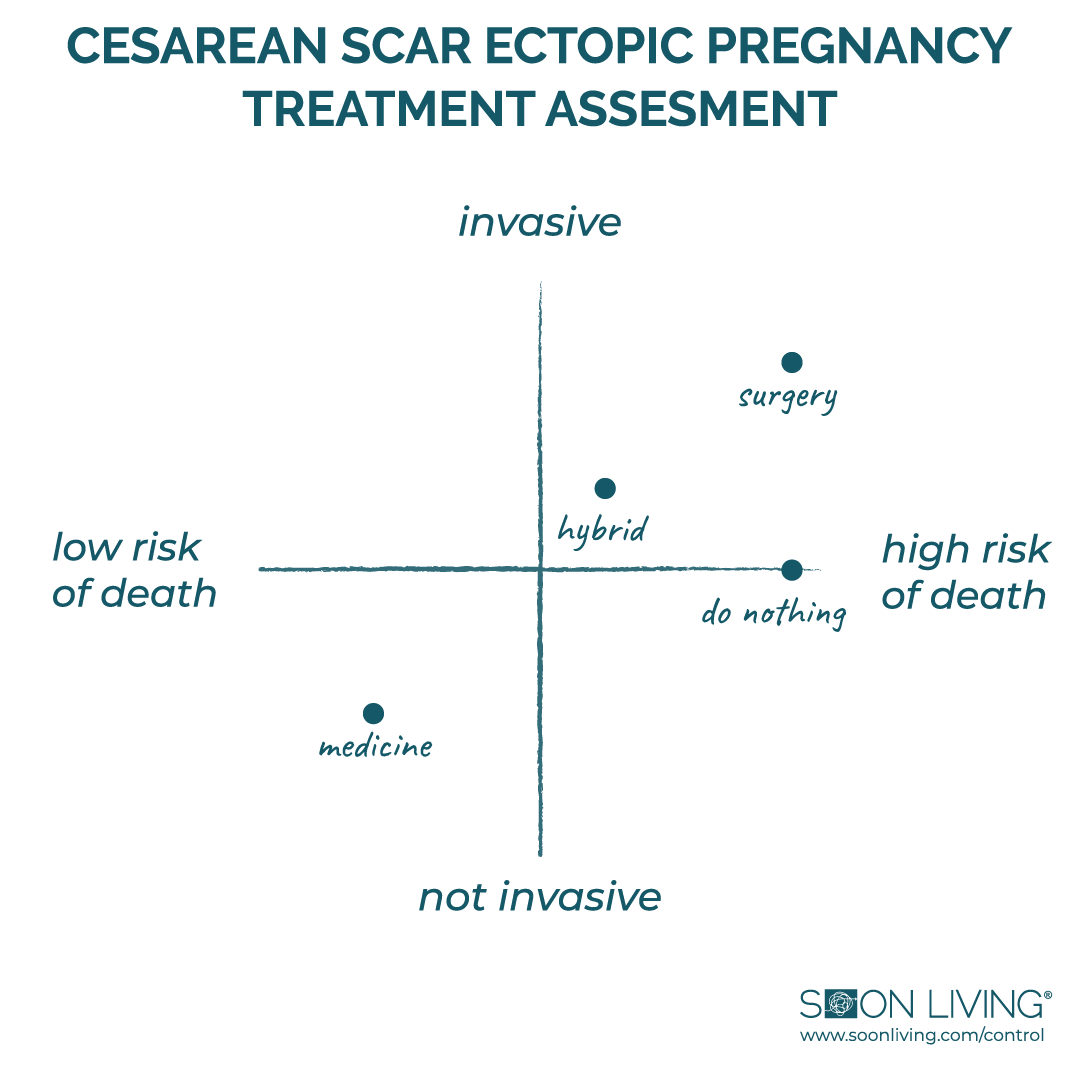
When I run out of analogies, I turn to visuals. I like things I can see, especially when they’re grounded in data. I remember picturing a scatter plot in my mind, trying to chart the variables — risk, invasiveness, outcome — anything to make the decision feel a little more rational, a little less like gambling with my life.
It was around this time that my husband called me back. His plane landed and he had listened to my message. I filled him in on everything I’d learned so far. I was still trying to wrap my head around it all, but saying the words out loud helped me process what was happening.
We agreed that not dying was the top priority. The scatter chart had helped us think through the data, science, and logic behind each option, and it was clear that medicine was the best path forward. I would review next steps with the doctor; he would start working on a return flight home.
–––––––––––––––––––––––––––
The doctor explained that their practice followed a multi-dose methotrexate protocol. It involved two phases and four steps.
How it worked:
Phase One: Active Treatment
Step 1: Establish a Baseline
What Happens: They would draw blood to establish an hCG baseline.
Why: hCG stands for Human Chorionic Gonadotropin and it is a hormone that is present during pregnancy. As a pregnancy progresses, it increases. Methotrexate stops the growth of the pregnancy growth, and declining hCG levels are how success is measured under this protocol. Every other day, I would return for another blood test to track the decline. My hCG needed to drop 15% or more from the previous measurement in order to move into Phase Two: Recovery.
Step 2: Administer Methotrexate
What Happens: I would receive two high dose injections of methotrexate and head home.
Why: Methotrexate is a chemotherapy drug commonly used to treat cancer, psoriasis and rheumatoid arthritis. It works by stopping cells from dividing, which is also what makes it effective in terminating an early pregnancy.
Step 3: Follow with Leucovorin
What Happens: The following day I would take a dose of Leucovorin Calcium.
Why: Leucovorin neutralizes the toxicity of methotrexate. Each time I received methotrexate, I’d follow with leucovorin the next day (completing one “round”). I’d continue this alternating schedule until my hCG levels dropped at least 15% from the last test.
When I asked how many rounds to expect, the doctor said there wasn’t enough data to know. When I pushed back, she suggested preparing for at least three rounds.
Phase Two: Recovery
Step 4: Monitor hCG Decline to Zero
What Happens: Once my hCG level reached the decline threshold, we would shift to the recovery phase.
Why: The protocol required ongoing blood tests until hCG reached zero. The schedule would move from every other day to weekly testing, continuing until my levels flatlined. I’ve since learned that, on average, this takes about 40 days.
While the process sounded simple enough on paper, I discovered that thinking about an abortion and actually having one are two very different things. One is hypothetical and the other is irreversible. This was a wanted child in an otherwise perfectly healthy pregnancy. It was an impossible decision. My focus became minimizing as much collateral damage as possible.
–––––––––––––––––––––––––––
When the nurse entered the room, I could only see her eyes. She was covered head to toe in what looked like, at the time, a makeshift hazmat suit.
2020 has brought a lot of things with it, including the knowledge that the nurse was actually just wearing standard Personal Protective Equipment [PPE]. Still, it caught me off guard, and I’m confident the shock showed on my face.
She explained that the PPE wasn’t to protect me but to protect everyone else. Methotrexate could be highly dangerous to the other pregnant women throughout their office. Even trace exposure could cause severe birth defects and/or fetal death. The PPE was a precaution against that risk, not against me.
I remember that sticking with me as I signed the consent forms. Then came the injections: one dose of methotrexate to each butt cheek and about 90 seconds later, it was over. I was 8w1d pregnant.
–––––––––––––––––––––––––––
1: Earlier in this section, I used a footnote citation. I’m including this note here so it doesn’t get lost at the end of the story.
Whenever I put something in quotation marks, it’s because I remember someone saying it that way — not because there’s a transcript, but because that’s how I remember it. Think of it as a narrative device, not courtroom evidence. I believe it is accurate but it is possible the other person remembers it differently.
For privacy and security, I’ve also chosen not to use anyone’s real name. If they decide to tell their version of events, I’ll link to it below. They’re also welcome to weigh in through the comments.
Thanks for reading this footnote — and for understanding the spirit in which it was written.
Quick pause for an important reminder about abortion legislation.
In 1973, the Supreme Court ruled that the constitutional “right to privacy” extends to a woman’s right to make her own reproductive decisions. But that right was never absolute — restrictions increased as a pregnancy progressed. Generally speaking, procedures before 13 weeks faced few limitations; between 14 and 26 weeks, they required medical justification; and after 26 weeks, abortion was prohibited except when the mother’s life was at risk.
From 1973 to 2018, the legal framework around abortion rights remained largely unchanged. But in just the past few years, a wave of state legislation has put those protections in serious jeopardy. Alabama banned abortion outright except to save the mother’s life. Georgia, Kentucky, and Ohio passed “heartbeat” laws prohibiting abortion after roughly six weeks — often before a woman even realizes she’s pregnant. Missouri followed with an eight-week ban.
Meanwhile, fourteen other states — including Arkansas, Florida, Iowa, Louisiana, Maryland, Minnesota, Mississippi, North Dakota, Pennsylvania, South Carolina, Tennessee, Texas, West Virginia, and Wyoming — have introduced or are considering similarly restrictive laws.
The stakes rose even higher when Justice Amy Coney Barrett was confirmed to the Supreme Court on October 26, 2020, just eight days before the presidential election. She is the fifth justice appointed by a president who lost the popular vote. #democracy
I am absolutely blown away by how significant the threat to maintaining the constitutional right to control one’s own reproductive decisions has become. I did not realize how many states and legislators were actively trying to restrict or outright eliminate it.
I’ll be honest: until my own experience, I hadn’t paid close attention to this debate. I grew up in a pro-choice home, in a state that has elected pro-choice governors since 1985. I thought the right to choose was settled law.
It’s not.
I firmly disagree with the opinion that government should have a voice in this conversation. I believe this is a basic human right — regardless of the circumstance. Having faced this choice myself, I understand just how complicated and heartbreaking it can be. And that’s exactly why I’m sharing this story — because no one should have to face it in silence or shame.
I was alone and emotional when I left my doctor’s office. I cannot imagine what that experience would feel like if it were bookended by pro-life protesters determined to create emotional and physical obstacles at every step. Torture probably doesn’t quite cover it. If you had to navigate something like that on top of the emotional rollercoaster that is abortion, I am so sorry that happened to you. If you haven’t — take 30 seconds to get a glimpse of their experience.
I spoke briefly with my husband on what seemed like the longest 15-minute walk to the ferry terminal. He was about to board his flight home. That was, by far, the best news of the day.
I quickly texted my boss [whom I had not yet told I was pregnant], to tell him I would be unavailable for the rest of the day due to a medical emergency. I said I would triage open items and follow up later in the week. I fired off a few emails, canceling meetings and letting clients and colleagues know I’d be out for health reasons until further notice. I hoped that would be enough to explain my absence (and prevent follow-up questions).
By the time I boarded the ferry (yes, that ferry — the one made famous by McDreamy, for my fellow Grey’s Anatomy fans), I was physically and emotionally exhausted. I headed straight to the bow. It was the only place that offered something resembling privacy; I could feel the ugly cry coming.
When I got home, all I wanted was to crawl under the covers and cry until my husband arrived. But when you have two kids under five, that kind of alone time doesn’t exist. With his flight and the commute from the airport, I needed a childcare plan to get through the next eight hours.
I gave our au pair a brief, high-level explanation and asked if she could shift her schedule until my husband returned. But I had forgotten she had school on Mondays and a hard stop at 4 p.m.
I quickly pivoted to plan B — my parents. Theoretically, this was a solid idea but my 70+ parents had their own long list of health problems. Running after active little humans was generally a challenge for them. I wasn’t convinced adding them to the mix would actually be helpful.
Even so, I decided beggars really can’t be choosers, ordered a pizza, and asked them if they could swing by to feed the kids dinner, watch them while they watched TV, and then help with the bedtime routine.
The pizza arrived before they did, which gave me time to rehearse what I was going to say. They didn’t know I was pregnant. After all, the last time we surprised both sides of the family—with a pregnancy announcement during family photos — I miscarried at eleven weeks and needed a D&C. That experience gave everyone a new appreciation for the phrase #AwkardFamilyPhotos. It’s also why we’d decided not to tell anyone about this pregnancy until the second trimester. At this moment, that decision felt wise.
Once they got settled, I uncomfortably shared the high-level explanation: “I have an extremely rare and potentially fatal type of pregnancy. None of the options are good, but the goal is to minimize risk and avoid death through several rounds of medication. I asked you to help with the kids because I had my first dose a few hours ago and I’m solo-parenting until bedtime.”
I could tell by my mother’s expectant grandparent glow that she stopped listening after I said, “I’m pregnant”. This was confirmed when she responded, “I’m so excited you’re pregnant!”
I took a more direct approach. I repeated myself—this time substituting “several rounds of medication” with “abortion.” The shock on her face confirmed that message landed. I wasn’t in the mood to help anyone else process my abortion, so I pointed out the pizza, turned on Peppa Pig, and ended the conversation by stating I was going to lay down and rest.
Quick pause to recognize my privilege in this situation.
This was a terrible experience. But it was made easier by the resources and support I had access to. I had a job I could step away from with a few emails, and a boss who was understanding and didn’t require follow-up. I had health insurance and paid sick leave, which helped minimize the financial impact. I had flexible childcare. And most importantly, I had people who showed up for me.
I know this experience would have been infinitely harder without any one of those things. If you went through an abortion without the support or access you needed, I am so sorry that happened to you.
I quickly learned that television doesn’t exaggerate the side effects of chemotherapy.
Nausea — check. Vomiting — check. Appetite changes and diarrhea — check, check.
By the time my husband got home, I was already in the bathroom, sick. I don’t have many clear memories between his arrival and our return to the doctor two days later, but I do remember the rhythm I fell into at home: it was basically bedrest and our 5ft x 5ft bathroom closet. With the exception of the occasional shower, I didn’t stray far from that circuit for weeks.

With hindsight on our side, we planned much better for Wednesday’s trip to the doctor. To avoid running into people we knew on the ferry — and to minimize the odds of an emotional breakdown in front of strangers — we decided to spend the extra $40 round-trip (plus $12 parking) to take the car. For perspective: minus the ferry, the trip was about a mile and a half. Under normal circumstances, the Jewish mother in me would never have approved that expense.
By the time we reached the exam room, my anxiety was off the charts. When my regular doctor walked in, her familiar face brought an immediate sense of relief. She was patient and kind as we peppered her with rapid-fire questions — many we already knew the answers to. Her calm energy brought harmony to our chaos.
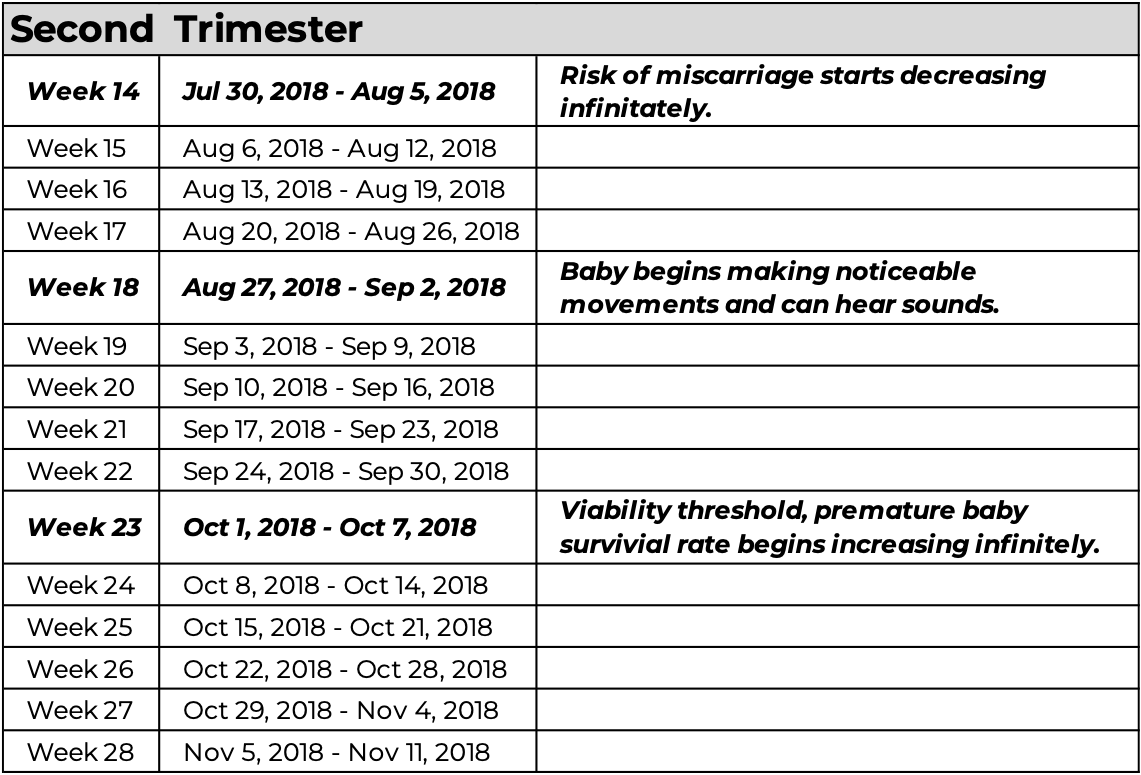
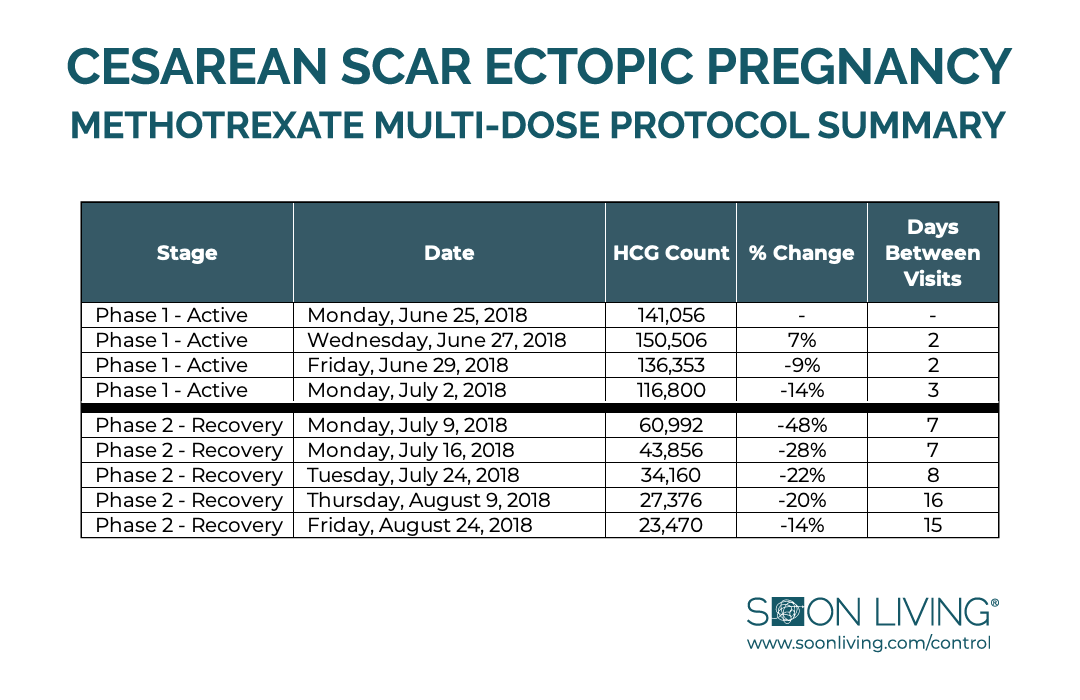
In total, I received four rounds of methotrexate before transitioning to the recovery phase.
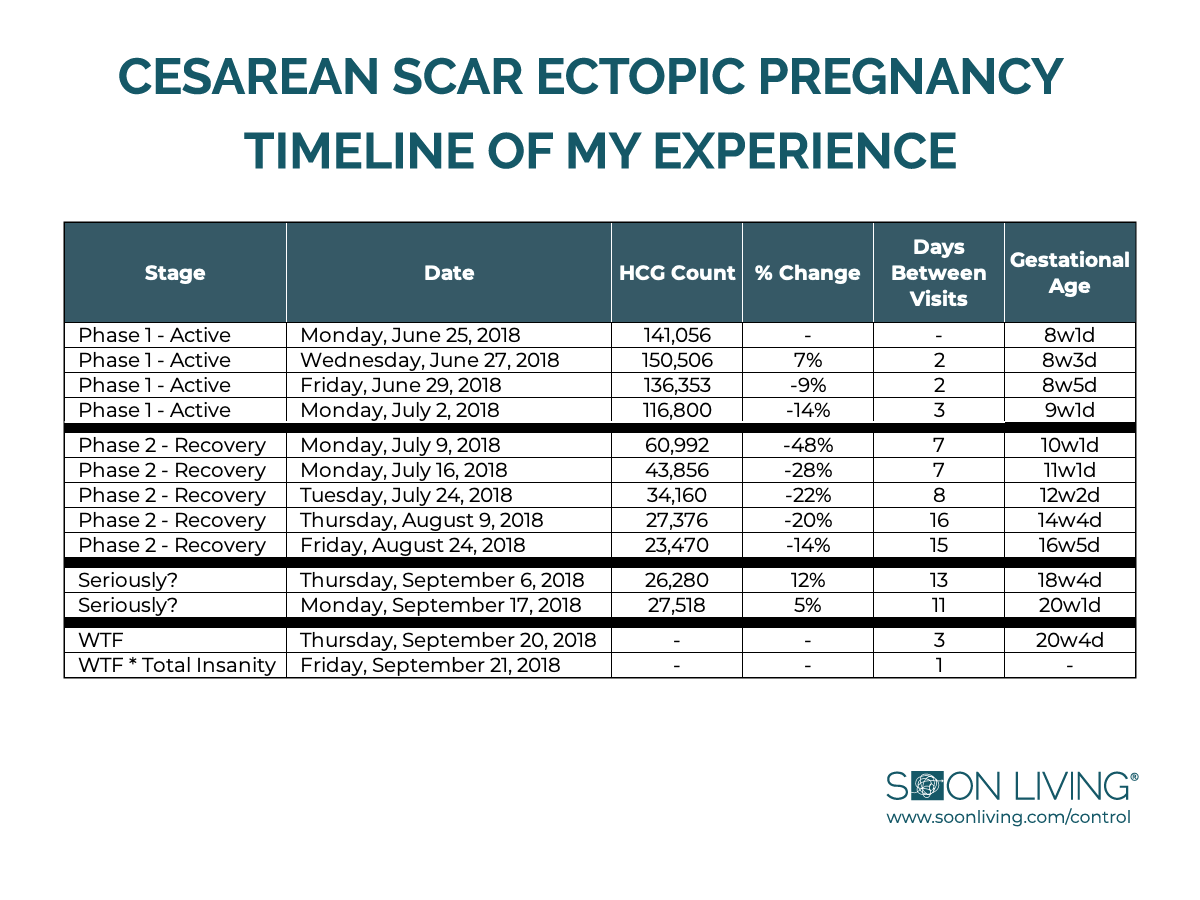
This chart summarizes the data behind that journey:
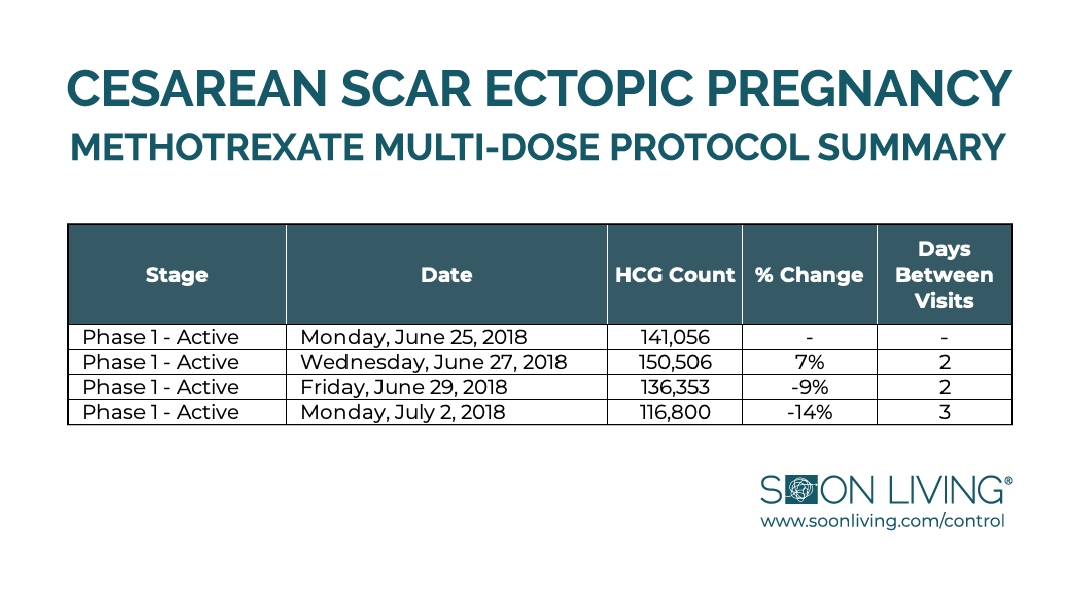
That last round on July 2nd was a real slap in the face. We had decided to push the hCG test out by one day since “every other day” landed on Sunday. I remember bursting into tears when the data came back showing I missed the 15% threshold by 1%.
I proposed rounding up, skipping the fourth injection, and calling it good. The doctor responded with a hard no.
What the chart doesn’t show is how miserable the methotrexate made me. As I mentioned earlier, I spent weeks cycling between bedrest and our bathroom closet — working my way through what felt like every side effect listed on the label. Nausea, stomach pain, no appetite, vomiting, constipation, diarrhea, fatigue, dizziness, drowsiness, chills, fever, headaches, mouth sores, bleeding gums, tender gums, you name it.
By the third round, I woke up covered in bruises. Worried, I called the doctor, who explained that in rare cases, bruising can be a side effect of methotrexate. Of course I was the patient lucky enough to win that lottery. I remember joking that if I had the same odds playing Powerball as I did medically, I’d be rich by now.
The chart also doesn’t capture the mental part of it. The anxiety. The depression. The night sweats and nightmares. One recurring dream put me in a red dress, on public trial, forced to wear the letter A — for abortion — then punished by Aunt Lydia in ways that felt too harsh for Hulu. #HandmaidsTale #ScarlettLetter
It’s safe to say it was rough. I wanted it to end. I wanted to move forward. I think, in hindsight, I understood that the “Recovery Phase” wasn’t just the last step in the methotrexate protocol — it was the first step in my actual recovery from this entire experience.
When the nurse in the hazmat-style PPE came in to give the final injection, I wanted to believe it would be the last time I’d ever see her in that capacity.
Quick pause to recognize those in my life who made the trek through chronic and/or terminal illness.
This experience gave me perspective — and deep empathy — for anyone who’s had to endure recurring medical treatment. I have mad respect for the people who do it while somehow maintaining a positive attitude.
My parents have faced more than their share: multiple sclerosis, stage 4 cancer, bipolar disorder, and chronic pain that led to battles with opioid addiction. I’ve watched friends and family navigate dementia, Alzheimer’s, Parkinson’s, brain tumors, strokes, and just about every variety of cancer.
These are the people who inspired me. Their strength, endurance, and determination were top of mind throughout my own experience. They taught me to focus on what you can control, and to do the best you can with what you have. I’m forever grateful for that wisdom.
If you’re in the middle of your own health battle, I’m so sorry you’re going through it. I hope that sharing what I learned from my experience helps you get safely to the other side.
I was beyond thrilled to move into the recovery phase on July 9th. I returned to my regular work schedule the following week but I was still pretty sick from the treatment. After a few very public moments that I’m sure people chalked up to morning sickness, my boss approved a temporary work-from-home-as-needed arrangement. It was a small change, but it made a big difference. He was very supportive.
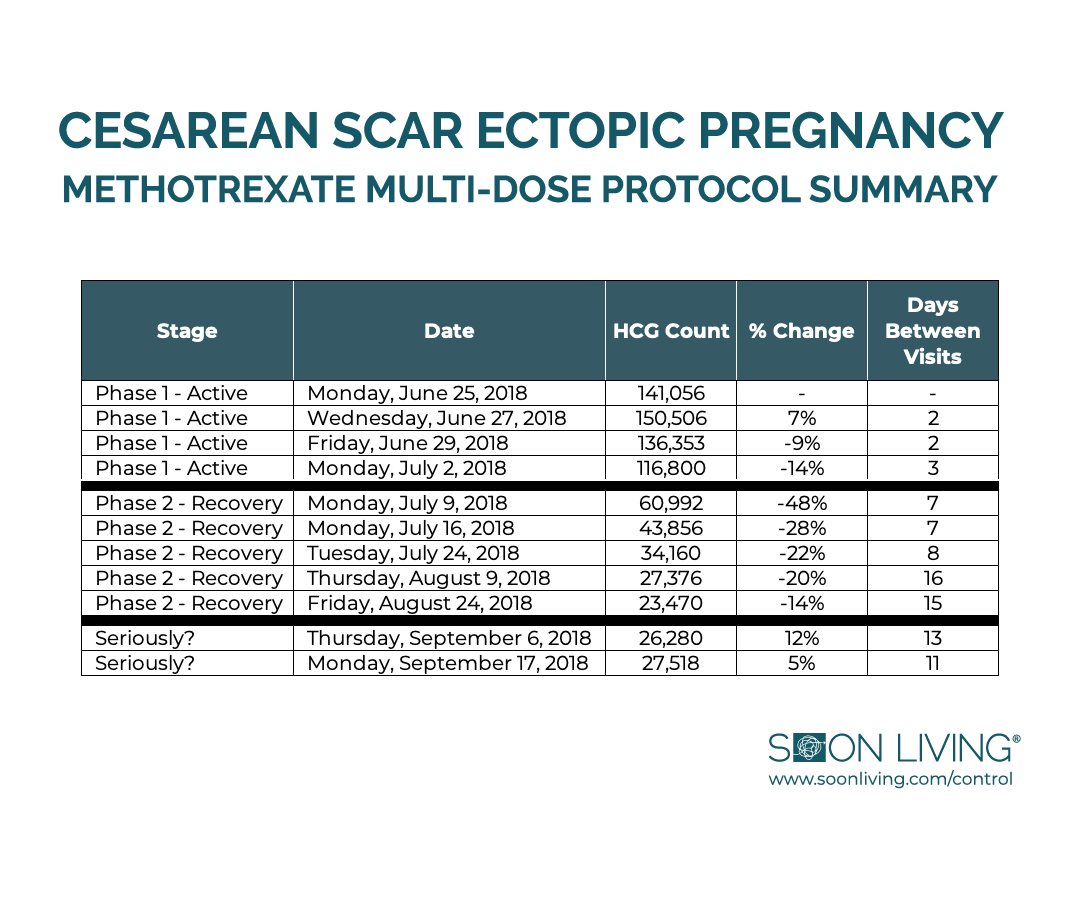
By the end of July the data indicated my hCG was on a consistent downward trend. To save me the hassle of schlepping into the city so frequently, we moved to biweekly hCG testing in August. Each day I felt a little better and a little closer to my regular self. This chart summarizes the data behind that journey:
Act Two: The Complication
Around Labor Day Weekend, everything changed. We were camping in the Olympic National Park where cell service was spotty. I initially ignored the voicemail message chalking it up to an appointment reminder. But when I finally listening, a day or so later, I knew the short and simple voicemail requesting I please call the office as soon as possible was really a clue that something was wrong.
Again, not a doctor — but I knew enough to know that when doctors need to deliver bad, unusual, or potentially dangerous news, they do so in real time and preferably in person.
When I called back, a medical assistant answered and told me she’d been expecting my call. [Also not a good sign.] She explained that my doctor was in surgery but had asked that I come in for an hCG check as soon as possible. I told her I was out of town and started asking detailed follow-ups. In my professional life, I facilitate interviews—we call this process “peeling back the onion.” She wasn’t prepared for that level of interrogation, and I got to the core pretty quickly: my most recent hCG decline had been smaller than expected. The cause was unclear, so they needed to recheck it. Since I wasn’t in immediate danger, we agreed I’d come in after returning from the trip.
A few days later, on September 6th, I found it difficult to hide my tears in the waiting room. I did not prepare properly for the emotional reaction that came from sitting in the middle of a room surrounded by other pregnant women. I tried to distract myself with my phone but suddenly found myself in the pregnancy tracking app I clearly should have deleted. Under other circumstances, I would be 18w4d pregnant with my third child. That fact was impossible to escape.
After a blood draw and another wait in a smaller room surrounded by instructional reproductive posters and gynecological training manikins, my anxiety was off the charts. I could sense the uncertainty when my doctor entered the room.
She was direct: my hCG levels had increased since August.
“Seriously?”
She was serious. She explained that the increase was an indication of growth.
Blergh. My mind was racing.
“What was growing? The baby? Was the baby still alive? How is that possible? Why is this happening? Did you know this was going to happen?” [I probably didn’t capture them all but you get the general concern.]
She explained that since cesarean scar ectopic pregnancies exist inside the uterus [where pregnancies are supposed to occur] and since my hCG levels had been declining as expected under the methotrexate multi-dose protocol, this was likely a sign that the placenta was still growing. While rare, the hypothesis was this was a completely reasonable explanation and the best next step was to resume the methotrexate multi-dose protocol immediately.
More tears. This was a real gut punch. I was just starting to feel normal again so the thought of getting back on the methotrexate rollercoaster was intimidating. After a few more clarifying questions, I understood that she did not believe my life was in imminent danger, and so I countered with a proposal.
I explained that after my 2017 miscarriage, I started a website [www.soonliving.com] to produce something productive vs. drinking a ton of wine and binging Netflix. Before this latest disaster, I had invested in web design training and an in-person conference which would take place in Florida from September 13th – September 17th. If we restarted the methotrexate now, I knew the side effects would sideline me.
“I need this,” was my closing argument.
She was quiet for a minute as I braced for more disappointment. To my surprise, she outlined her terms: if I came straight to the office from the airport after returning home from the conference and if I promised to seek immediate medical attention at any sign of fever, abdominal cramping, and/or bleeding then she would not object to my attending the conference.
I agreed to her terms and left quickly before she changed her mind.
Act Three: No Turning Back
The Activate: EBA Live conference was incredible. I met hundreds of other bloggers, learned a ton of best practices and heard some pretty inspiring stories.
One that stuck with me came from Abby Rike Rockenbaugh, who shared how she lost her husband, daughter, and newborn son in a car accident while she was at a doctor’s appointment. She spoke about the deep depression that followed, her journey through The Biggest Loser, and how she eventually turned tragedy into something meaningful — a way to help others through their own darkest days. I’ve thought about her story often since that trip. She’s one of the reasons I was able to anchor myself in this crisis.
As promised, I went straight to the doctor’s office after my flight from Orlando landed. I already knew my regular doctor was out, so I wasn’t surprised when another physician came in to review the results of my latest hCG test.
She explained that while the change was small, my hCG had increased again — now higher than it had been in early August.
“Seriously?”
She was also serious. Same talking point as before: this is a sign of growth. She reiterated how important it was to resume the methotrexate protocol immediately.
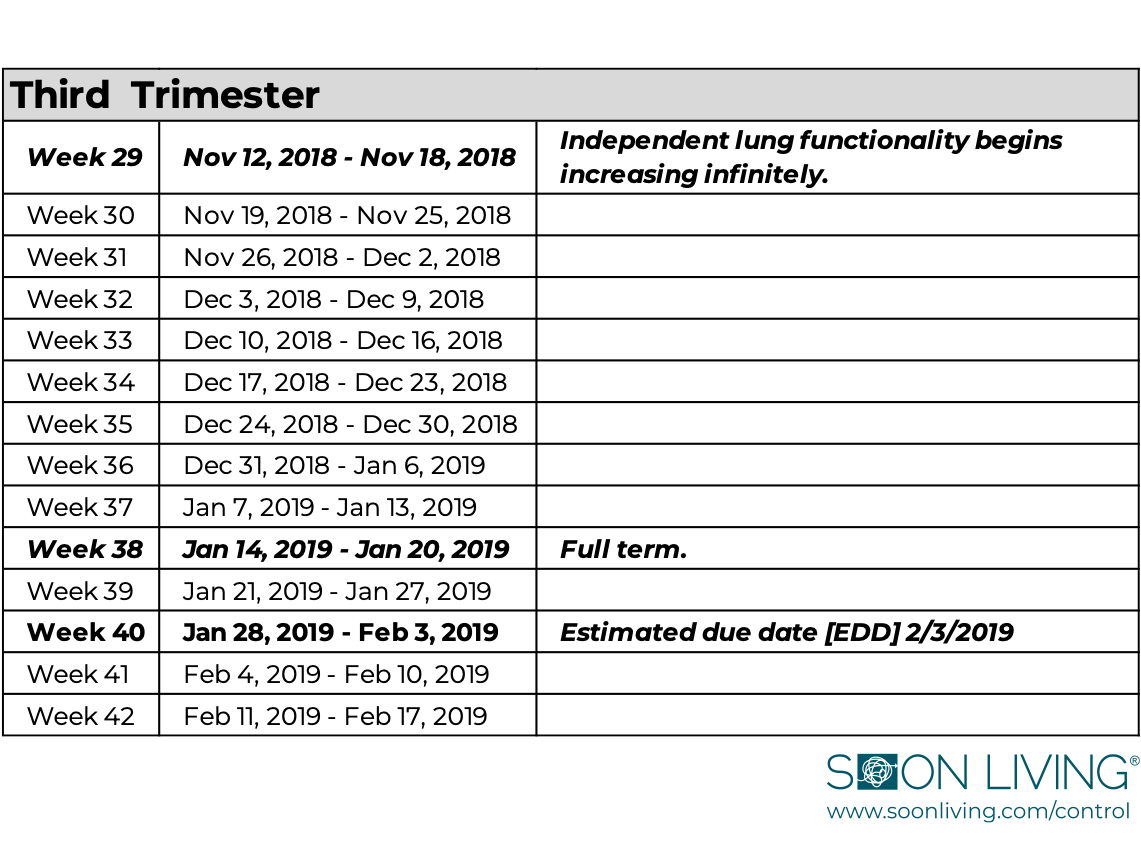
This chart represents that data:
That definitely killed my conference high. I immediately became nauseous thinking about the obvious question: How sure are we that the baby isn’t what was growing? I asked the doctor to help me understand what, exactly, was happening inside of my body.
She reiterated the working hypothesis — that after all the methotrexate I’d received, it was most likely the placental tissue that was still growing. Then she mentioned she’d once had another patient with a cesarean scar ectopic pregnancy whose hCG had also spiked after a steady decline.
That got my attention. I’d never actually heard about another patient in real time. This was one degree of separation, and I suddenly had about 10,001 questions.
She emphasized how rare it was, but said that in that case, a second wave of methotrexate resolved the problem after two additional rounds. I thanked her — the information gave me a way to set expectations for what might come next.
She was almost out the door when I stopped her.
“Why haven’t I ever had another ultrasound to confirm that the treatment was effective?” I asked. “I’ve been having these awful dreams about slowly torturing my child, and now, with this new information, it’s hard to ignore them. Is it a cost thing? Or because whatever shows up on the screen would be… disturbing?”
She seemed surprised by the question. She simply reiterated that we were following the methotrexate multi-dose protocol and that and that post-treatment ultrasounds weren’t part of the process.
Not being a doctor, I didn’t push back. She left and a few minutes later the nurse in the hazmat style PPE came in to give the injection. I was out the door two minutes later, headed home to brace for the disaster I knew was headed towards me.
About 10 minutes later, I was surprised to see an incoming call from my doctor’s office. It was the doctor I just saw. She said she’d spoken with my regular doctor, and together they’d decided I should, in fact, have another ultrasound. She asked me to call the out-of-network specialist to schedule it.
–––––––––––––––––––––––––––
The first available appointment was four days later. It was a bit of déjà vu but I tried not to think about that.
By the time I got to the exam room, my anxiety was out of control. When I’m nervous, I talk a lot. It’s a coping mechanism. Sometimes I just share personal details about myself or my family, other times I ask a lot of questions. In this appointment I did both.
I started by asking the ultrasound tech if she had ever seen a cesarean scar ectopic pregnancy. She had, once. When I asked what happened, she explained that their office handles high-risk and unusual pregnancies, drawing patients from all over Washington, Alaska, and parts of Idaho.
The woman she mentioned had lived in rural Idaho. Her local doctor suspected a cesarean scar ectopic pregnancy and referred her to Spokane. That doctor confirmed the suspicion and referred her to this Seattle clinic. “It’s a rare diagnosis,” the tech said. “That makes doctors nervous — they want to pass the case to someone more qualified. But we were the third place she had to go before getting answers. What a terrible experience for her.”
That resonated with me. 1000%.
When I asked what happened next, she told me the diagnosis was confirmed late in the pregnancy. The team terminated immediately using a potassium chloride [KCL] injection directed into the fetus’s heart, followed by surgery that ended in a hysterectomy.
That struck me hard, like lightning. I looked her in the eye and said my own journey had been long and confusing — and that whatever she found, I wanted the truth.
She nodded and then started the ultrasound. I was babbling on about my conference in Florida and a recipe I was about to publish, when she interrupted me.
“Remember earlier when you asked me to be straight with you?” I nodded.
“I’m sorry to tell you this but the baby still has a heartbeat and I need to step out because I honestly don’t know what to do.”
“What the fuck.” [We are at the point in the story where I start swearing profusely.]
She apologized again and left the room. I immediately called my husband. His reaction matched mine — swearing, confusion, disbelief. For the next five minutes, I cycled between rage and self-blame, trying to make sense of the impossible.
When the tech returned, she brought a doctor. They’d spoken with my doctor’s office and wanted to gather more images before deciding next steps. “We’re working on a plan,” the doctor said.
Sure. That made sense. [I actually don’t think I responded.]
The doctor left, and the tech resumed scanning. I was in shock. I remember very little. She called the doctor back in once or twice, clearly unsure of what to do. It was obvious neither of them knew.
At some point, it occurred to me ask the obvious question, “How far along am I?”
“20w4d based on your LMP…but the baby is measuring at 17w3d.”
I didn’t know what the fuck that meant. I understood “20-weeks” and “LMP”. That was how we dated my other pregnancies — and by that math, I was at the midpoint.
“Unfuckingbelievable.”
After the scan, the doctor returned to say that my doctor’s team was still “working on the plan,” and that I should head home and wait until they called.
“Home, home?” I asked. “Like make the 45-minute ferry commute home and wait there, or leave this office and don’t yet go to the other doctor’s office, but stay close by in case there’s an emergency while “the plan” is being finalized?”
It was the latter.
I texted my husband to tell him the very unhelpful update, and then immediately called my aunt — who is an actual doctor. I felt like I was standing in the middle of a Grey’s Anatomy episode, both literally and figuratively, since I was still at a hospital in Seattle. I knew I could count on her to tell me what the fuck was actually happening.
She picked up right away but told me she was about to go into surgery. I gave her the high-level summary. She was calm and told me she’d call me as soon as possible.
I wasn’t expecting that. Now I was standing on the street. Next to the hospital. Not really sure what to do.
I started to panic. My heart was racing. I got really sweaty, and dizzy, and started hyperventilating. Then I made it worse by trying to figure out if what was happening was an actual panic attack or something worse. I sat down on a bench to do some deep breathing. Something I picked up from one of my medical dramas.
It worked.
I’m not sure how much time actually passed. But then I realized that my brother was the only other person in the city I felt comfortable calling. I texted him, “Call me immediately.”
He called me back within 30-seconds. It was a surprise, cause he is my younger brother, and he is usually not that responsive. I think that is why I started the conversation with, “I’m surprised you called me back so quickly.”
He explained that I’d never texted him to “call immediately” and so he thought that meant one of our parents had died.
“Fair assessment. They’re fine.”
Then I told him the problem wasn’t that someone died — it was that they didn’t. I had just found out I was still pregnant and was standing outside a hospital waiting for doctors to figure out what to do next. I was hysterical; I’m not even sure he understood me. He told me to text him the address and said he’d be there right away.
Quick pause.
I later found out he was actually in the middle of leading a meeting when he got the text. He saw it, finished his sentence, and said he needed to step out for a minute to check on something. We spoke. He came back in. Told everyone he was ok but there was a family emergency, and that the meeting was over. He picked up his computer and said he would check back in when things were under control. Then he left.
His behavior is absolutely what you should do if someone you care about asks you for help with their crisis. It feels like this should be obvious but 2020 has made me question a lot of things that humans do or don’t do. So I felt it would be a miss not to point this out.
The next call I got was from my doctor. It was her day off but her colleague, the doctor I’d seen on Monday, had caught her up on the ultrasound results. I asked her to help me understand what was happening and why. She stated that it was a complete shock not only to her, but to her entire medical practice.
I told her I was literally standing on the street outside the hospital and needed a plan: Should I go home? Should my husband come to Seattle? Did she have any sense of what the plan might be? A timeline? Anything?
There is a lot about this day that I wish I could remember to forget. Her response was unfortunately one of those things I will always remember. She said that she was, “consulting with experts across the country on treatment options.”
It’s not a good sign when your doctor tells you they aren’t exactly sure what to do next. I rephrased the question, “Am I going to die?“
She assured me I was not. She told me this was completely unexpected, that they hadn’t been able to find any other reported cases like mine, and that—despite the shock—I essentially had three options:
Option #1: Continue with the Pregnancy
I don’t remember my exact reaction but I definitely swore, a lot.
This is not verbatim but it was something like, “Seriously? If that’s the first option then I’m going to need you to help me understand why the FUCK didn’t we choose to do that in the first place? Especially considering we spent the last 12 weeks navigating to this shitshow. Also, what kind of baby is going to come out after hazmat lady injected toxic medicine into me — not once, but FIVE FUCKING TIMES!!??!!!“
She kindly absorbed my rage and acknowledged my questions were valid. She explained that based on the gestational age, and her commitment to transparency, she needed to present every possible option.
She confirmed that all the original risks were still on the table: uterine rupture, catastrophic hemorrhage, blood transfusion, hysterectomy/loss of fertility, and death. And given the heavy, repeated exposure to methotrexate, the likelihood that the baby would survive was essentially nonexistent.
I’ve had a lot of time to reflect on this story and this moment is the best example I can highlight of patient/doctor trust. My doctor is the kind of doctor who makes medical recommendations independent of her own religious beliefs. That matters. Mixing religious ideology with science and medicine is dangerous. If you want patients to trust their doctors, those two things must remain separate.
I said no; next option.
Unfortunately, when I learned about the remaining two options, it became painfully clear that not everyone in the hospital’s medical hierarchy shared her commitment to keeping religion out of medicine.
Option #2: Surgery
She explained that the ultrasound raised serious concerns about the thickness of my uterine muscle. It also showed placenta previa — the placenta was covering the cervix. Combined with two prior cesareans and the cesarean-scar ectopic pregnancy, the working hypothesis was that I might also have placenta accreta.
For context: with accreta, the placenta doesn’t just attach to the uterus — it grows into the uterine wall. And when you try to detach it, you can’t. Not without a hysterectomy.
A hysterectomy was so final. Too final.
I asked her to tell me about the third option.
Option #3: Alternate Plan
This option was still surgery—and it would only work if I did not have placenta accreta. The idea was that she would deliver the baby similar to a standard cesarean. If preserving my fertility was a priority, this was the only surgical option that offered even a possibility of that outcome.
I fired off a few technical follow-up questions, and I will never forget her response. She said she didn’t know, “not because as surgeons we can’t do this surgery but because this surgery has never been performed.”
That took my breath away. It was also, in a twisted way, that Dr. Addison Montgomery-Shepherd moment I had been looking for earlier. Except it was immediately clear that I would have preferred to watch it unfold on any literally any show vs. it being one of my only three options.
I asked if this option put my life at any additional risk. It didn’t. Mainly because if they found an accreta once they were in surgery, they would immediately pivot to Option #2 and perform the hysterectomy.
Based on that, I chose Option #3. Then I asked what came next.
There were a lot of really shitty parts to this day. This next part is the third shittiest. Consider this your warning label.
My doctor took a deep breath, as if reminding herself to strip away her personal feelings before speaking. She explained that because the hospital was owned by a Catholic institution — and because the baby’s gestational age was now well into the second trimester — I could not enter the operating room with a fetus showing cardiac activity.
She acknowledged how absurd this was, especially in my use case. My life was at risk. The baby’s chance of survival was essentially nonexistent. But the hospital followed a Catholic directive that prohibited intentional second- and third-trimester abortions.
As a result, before surgery, I had to go back to the same out-of-network ultrasound specialist for an ultrasound-guided KCL injection delivered directly into the fetus’s heart. That would stop the heartbeat. She wanted me to have the injection that afternoon while she worked on booking an operating room for either immediately afterward or early the next morning.
If you were curious, it registered immediately. The next step in this horrendous nightmare was to watch someone insert a long needle through my abdomen, into my uterus, and into my baby’s heart — so they could inject a chemical solution designed to kill my child. #LifeGoals
“I’m going to need a Xanax,” was, I believe, my official response. I was overwhelmed, and that was the only sentence that made it out of my mouth. I’d never taken Xanax before; I only recognized it from television.
By then, my brother had arrived. We agreed that I’d hop in his car and head to her office. Since Xanax was a controlled substance, the pharmacy required a physical prescription. We’d pick it up, and she would work on scheduling the KCL appointment.
No recollection of the drive over to her office whatsoever. My brother offered to go inside for the prescription while I stayed in the car. Good call — I couldn’t imagine keeping myself together in that waiting room. While he was gone, I called my husband to recap the plan. He would coordinate childcare, pack a bag, take the next ferry, and meet me at the appointment. My job was to text him the time and location.
When my brother returned, he showed me a sticky note with the appointment time. We had 90 minutes. We started by getting the prescription filled.
I’ll be honest that the next 90-minutes are a blur. Part of that was the Xanax, part of that was that I just let my brother do everything for me. I remember going through the motions: parking, pharmacy [drop off], Espresso Vivace [waste time], pharmacy [pickup], parking at the medical building, elevator, waiting room, sign consent forms, wait. I feel like it’s the closest thing I’ve had to an out-of-body experience.
I felt instant relief when my husband entered the waiting room. My brother is a great support person, but he was not my husband. The three of us went back to the exam room together.
Then it was like we got the band back together. Same ultrasound tech. Same doctor. #JamSession
The doctor explained the procedure. It sounded simple and straightforward but also felt like such unfortunate déjà vu. Here I was again at the crossroads of thinking about an abortion and actually having one. Only this time it just felt like everything was collateral damage. I wanted it to be over quickly.
The doctor asked if I wanted to close my eyes or look away. I did but I wouldn’t. I decided that if the baby could make it this far – through 20 weeks of pregnancy and five rounds of methotrexate, then the least I could do was be present for the end.
So I squeezed my husband’s hand and sobbed. Then I watched her insert the long needle into my stomach, through my uterus and into my baby’s heart. I squeezed his hand tighter as I watched her inject the medication.
But nothing happened. I could tell immediately that wasn’t the outcome she expected.
She reloaded the syringe and repeated the process.
Still nothing. She awkwardly excused herself and left the room. I remember thinking, “is this normal?”
It wasn’t. But I’d been swimming in abnormality for so long — at this point, what was?
She came back and loaded the syringe again. Seriously? Three times? That was the second shittiest part of the day.
She tried again. We waited. Then she said, “That was it. That’s the money shot!”
That was undoubtedly the shittiest part of my day. Obviously because I just intentionally killed my child. But also, who says that? She did. I checked. Both my husband and my brother confirmed. It was not the Xanax. It was wildly inappropriate. I do chalk it up to nerves. Or bad training? It’s probably pretty rare that a guided ultrasound KCL injection requires three rounds. I imagine they don’t plan for that scenario — let alone provide coaching on how to navigate it properly with a patient.
Another blackout. I think my brain just couldn’t handle anything else. They put me in a wheelchair and the doctor escorted us across skybridges and through two or three medical buildings. She took us into the main hospital. Then to the Labor and Delivery wing where they put me in a room that looked a lot like the other ones I’d been in before.
That was different. That was beautiful and filled with the joy of becoming a parent. This was sad and filled with immeasurable grief that I wouldn’t wish on anyone.
At some point, another doctor came in and told me surgery was scheduled for early the next morning. She would be one of the surgeons, along with my regular doctor and others. They would walk me through details in the morning. For now, they would admit me overnight as a precaution, in case they needed to intervene urgently. She suggested I rest.
Then my aunt showed up. I had totally forgotten about her! My brother must have been coordinating everything behind the scenes.
The three of them made a plan:
-
My husband and brother would return home for the night.
-
My brother would help with the kids and pack essentials.
-
They’d bring the kids in the morning so we could see each other before surgery.
-
The kids would stay with my aunt and uncle for the weekend.
-
My brother would support my parents through their fear and confusion.
At least, I think that’s how it happened. I was definitely on drugs. Between the Xanax and some unexpected pain meds, I don’t remember much else until the next morning.
When I did wake up, my mind was very clear. Clear enough to confront the last twelve weeks.
And as someone who loves a visual aid, I updated the chart to include gestational age. It made something painfully obvious:
The baby was with me at every step of this very unfortunate journey.
Now — here’s why I bothered with that origin story. You don’t get a cesarean scar ectopic pregnancy without a cesarean scar. And in my case, that scar wasn’t the result of an elective birth plan; it was the life-saving solution to a very real, very serious problem. I don’t remember much about what happened next. I know alarms were ringing, a nurse came in, more medicine happened, and eventually I calmed down.
This was great timing because my kids arrived shortly after that. We read books and drew pictures in between various doctors popping in to prep me for surgery.
When it was time to head to pre-op, I could only take one support person. Obviously, I wanted my husband. I assumed he’d brought the Au Pair with him for this exact moment. He had not. He explained that she’d only been living with us for 12 days and he didn’t want to terrify her. Fair enough.
Tough to say who looked more shocked — my husband when he realized he hadn’t thought through this part of the childcare plan or my brother when it became clear that he was suddenly in charge of two small children. Either way, it brought me a little humor.
I was pretty stressed about the surgery in pre-op. When I’m stressed, I like to get organized and make detailed plans. It’s a coping mechanism. I think it gives me a sense of control. Unfortunately, it’s the opposite of what my husband likes to do in this type of situation. So suddenly trying to organize finances and make an outline for what he should do in case I died — well, it was not helping him stay calm.
–––––––––––––––––––––––––––
The next thing I remember is my husband consoling me in my hospital room. Several hours had passed and the surgery was over. Apparently, I was inconsolable in post-op when they told me the only viable option had been a hysterectomy. My husband explained that it took a while for me to accept the news.
At some point, my doctor came in to check on me. She told us about the surgery. Overall, it went well. There were three surgeons, an anesthesiologist, a scrub nurse, and a circulator nurse in the room. They quickly confirmed placenta accreta. The placenta had grown through the wall of my uterus but had not invaded my bladder or blood vessels. That was incredibly lucky; the hysterectomy was unavoidable, but it could have been so much worse.
Then she explained something called a “uterine window.” There was essentially no uterine muscle covering the amniotic sac — the uterus was already separating or in the process of rupturing. In other words, uterine rupture wasn’t just possible, it was imminent. Operating when they did likely saved my life.
Then I asked her about the baby.
She told us it was a boy. She explained that the effects of the methotrexate multi-dose protocol were unmistakable — the birth defects were severe. Worse than anything she or the rest of the team had seen. His body was already undergoing fetal pathology, a diagnostic process used to examine congenital abnormalities. The hospital would create the formal pathology report to document the “fetal demise,” a medical term I wished never became part of my vocabulary, and then his remains would go to the children’s hospital for deeper evaluation by pediatric specialists. She warned me I’d likely receive automatic notifications as the reports were uploaded. She didn’t want me blindsided.
She also gently told us that some parents find value in seeing or saying goodbye to their baby in later pregnancy losses. Because of the logistics of my surgery, that wasn’t possible. She had photographs, but they were graphic and painful. There was no rush. The decision was ours.
I appreciated how human she was with me. She treated me like a person, not a complication. It took me back to the first day we met — when I had gone into labor unexpectedly with my first child.
Adding a stranger to the already unstable environment of first-time parenting can be tricky. We met, exchanged the bare minimum of introductions, and then she calmly announced that we’d be heading to the OR for an emergency cesarean. No preamble. No gentle ramp-up. Just: your baby is breech, this is dangerous, we need to move now. Instead of head-down, our baby’s butt was in its place. The risk of getting stuck and jeopardizing both of us was very real.
What struck me instantly was her delivery: direct without being cold, empathetic without losing authority. She had that rare blend of confidence and humanity you hope for when you’re terrified and seconds away from major surgery. She didn’t sugarcoat anything, and she didn’t dramatize it either. She simply told the truth, and guided us through it. That balance of empathy and competence was exactly what we needed to steady ourselves in the swirl of fear, uncertainty, and doubt.
That’s why I chose her as my primary doctor in my second pregnancy. And why I followed her to a new practice for my third. And why she ended up guiding me again through this final pregnancy/calamity.
Now. Here’s why I bothered with that origin story. You don’t get a cesarean scar ectopic pregnancy without a cesarean scar. And in my case, that scar wasn’t the result of an elective birth plan; it was the life-saving solution to a very real, very serious problem.
According to the CDC, in 2018, about 1.2MM US deliveries — 32% — were via cesarean. When I see that number, two questions haunt me: 1) How many of those 1,208,176 women will learn about a cesarean scar ectopic pregnancy and all the impossible decisions it forces? 2) Is there anything I can do to help them?
In total, I stayed in the hospital for a week recovering. Quick shout out to all the doctors and nurses who worked on this case from start to finish. Your care and compassion made a significant difference — thank you.
My husband stayed home with the kids because seeing me in the hospital scared them. I didn’t want to be alone, so my aunt stayed one night, my brother stayed two, and then my oldest friend flew across the country and slept in a hospital recliner for three more. I will never forget that.
I had a lot of visitors in the hospital. There was a lot of family. They even organized a birthday party to celebrate my son’s 3rd — as his planned celebration had been abruptly canceled for obvious reasons.
Friends came…Childhood friends. Adult friends. Work friends.
About halfway through the week, one of my closest friends visited. She surprised me when she shared that she just recovered from her own terrible pregnancy crisis. Her baby had anencephaly — which is a rare birth defect that impacts brain development. This too was a popular storyline across medical dramas, but I didn’t share that. Instead, I listened as my friend walked me through her crisis. How there is no cure and that babies born with the condition are either stillborn or typically survive hours to days following birth. She told me about when they found out. That the gestational age was right at the cutoff. They didn’t have a lot of time to decide. In the end, she she chose to abort — one more week and she would have had to take the baby full term. “It was hard. That would have been so much harder,” I remember her saying.
I think about her all the time when I think about abortion legislation — how a different ZIP code, a different state legislature, could have stripped her of the only humane option she had.
–––––––––––––––––––––––––––
One of my friends set up a Meal Train before I even got home. The meals were very helpful and a huge thank you to the dozens of friends, neighbors and acquaintances who dropped something off.
Then there were more visitors. Some with food. Some with flowers. Some listened. Some shared their own stories. Stories of loss. Stories of tough choices. Secret abortions that they never told anyone about until now.
It took me about six weeks to recover physically. My employer ended up processing the leave of absence request as a maternity leave. Not only did this mean that I had a generous amount of time to recover, it was also completely paid per a recent maternity leave change policy. Whoever you are, in Benefits or Human Resources: thank you. Not only was that the right thing to do; it was the human thing to do and I will forever be grateful. Ironically, this was the longest time I had ever received of paid maternity leave. With my first two children the benefit extended eight weeks. I am so happy that my company recognized new parents need more time.
–––––––––––––––––––––––––––
As long as this story is, the time has come to bring it to a close. I do want you to know that being able to talk about it, out loud and on the internet, did not happen overnight. It took months of reflection, and therapy, and tears, and wine. Most of all it took time.
One last visual aid — these are pictures of my family planting a tree.

The folks at The Living Urn made it very easy and our Willow Tree arrived quickly. We call it the Noah tree because that is what we decided to name him. For two years, Noah sat in an urn on the bookshelf in my bedroom. I put him there intentionally so that I could think about his journey. His tenacious spirit. But most importantly, to think about how he is someone who I would never get an opportunity to fully know.
2020 has been a year unlike anything I ever imagined. But as we approached September, something felt different. This year, I had enough emotional clarity to be ready to move forward. And so one fall afternoon, we dug a hole as a family and honored Noah whose name means peace and rest.
–––––––––––––––––––––––––––
I honestly don’t expect people outside of my family and friendship circle to read this. For those who do, I will be curious to learn how many make it to the end. If we haven’t spoken in a while — feel free to drop me a line. I’d love to catch up.
For anyone still with me, I want to leave you with this. Another very important lesson this experience taught me was how to move ahead after surviving a crisis. I tried a lot of different strategies but the one thing that got me to today was simply: start where you are and try to move forward, just a little bit, every day. #control
Epilogue
What mattered was her courage—sharing pain that raw helps people. It helped me.Alright. It’s Friday, October 30th. The year is 2020. We are deep into a global pandemic. In four days, I will have voted in my 7th presidential election.
I’m telling you this because the election is what prompted me to write this story and share it on the internet. This was after a friend passed along Haylie Grammer’s story — a woman in Texas who had to make a similar tough decision for her baby at 25 weeks.
She decided to tell her story because she read about Michigan Senator Gary Peter’s experience. He’s the first sitting senator to openly discuss his child’s abortion. The decision to share came in the middle of his own election cycle.
Then I came across Rabbi Jaclyn Cohen’s abortion story. She didn’t just defend abortion as a right; she highlighted the truth that women of every background, economic status, and faith have them. It was grounding. It was human.
I then learned about Chrissy Teigen and John Legend’s pregnancy loss. [I fan over them both.] She first posted about it on her social media and I remember thinking of how hard it would be to go through something like that on the world’s stage. I admired her strength and was inspired by her willingness to openly share the vulnerability. Four days ago, she published an essay detailing her experience and describing her loss. I learned that she lost her baby, also a boy, at 20 weeks like I did. She never used the word “abortion” and she didn’t need to. It was her story, her child, her grief. What mattered was her courage, sharing pain that raw helps people. It helped me.
And then came the final straw.
It was this piece of legislation from Ohio that was co-sponsored by 19 Ohio legislators. It proposed doctors be required by law to “reimplant an ectopic pregnancy into the woman’s uterus.” The bill went on to outline that those doctors who did not comply would face criminal charges.
To be clear, so there is no confusion down the line — this proposed procedure is not medically possible.
There could not be a better example for why politicians should be prohibited from creating laws about things that they do not have experience with or expertise in. If reimplanting an ectopic pregnancy was medically possible, I’m confident I would have chose to do that instead of the nightmare that I’m often surprised I actually lived through.
It was for this reason, writing became my top priority over the last 12 days. I took time off from work, have been sleeping very little and at times am so focused on publishing this story before November 3rd, that I forget to shower or eat. I haven’t worked this hard on anything since college. The stakes are much higher than finishing a term paper I had procrastinated on all quarter.
Quick pause for a review of presidential elections in the last 20 years.
It recently occurred to me that 20 years ago I voted in my very first Presidential election. The other guy won after some craziness with hanging chads and a Supreme Court ruling. He became the first president in my lifetime to win the presidency after losing the popular vote. The second guy to do that is our current president. That means that in one-third of the elections I have voted in, the candidate that became president failed to secure a majority support from voters. Those two presidents then turned around and appointed five of our nine sitting Supreme Court Justices. For the rest of their lifetime, those nine people will make decisions that impact everyone in our country. That’s insanity, not democracy.
And it’s also something I cannot directly control.
What I could control was trying to reach the undecided voter. It has been a popular call to action across all social media channels for weeks. Connect with undecided and/or Republican voters and do whatever you can to convince them they should vote for Biden. Tell them human rights are on the line. Make them understand that four more years of the other guy will probably mean the beginning of the fall of the American Empire. Or at least that’s what they will teach future generations when they examine the last 20 years of American history. Assuming we have a future — given that the earth is dying and our current president believes the environment is in the way of making money vs. recognizing that humans should partner together to save the environment while also making money from that effort.
Exactly eight weeks ago, I had spinal surgery. The reason is not important right now. What is important, is that exactly two weeks later, Supreme Court Justice Ruth Bader Ginsburg died. Since I was in the thick of my recovery, I had a lot of extra time to binge watch television. When the home screens of my favorite streaming services started promoting RBG and On the Basis of Sex — I decided to give it a go. I now understand the incredible impact Justice Ginsberg had on equalizing opportunities for everyone. I’m just sorry I never had the opportunity to let her know how grateful I am for that support. #NotoriousRBG
That led me to discover Mrs. America which was an excellent examination of the battle to move the Equal Rights Amendment across the finish line. I finished that in two days.
I sensed my husband was feeling left out of my streaming party, so one night we watched our first movie in months — Jon Stewart’s Irresistible. Highly recommend — it opened my eyes to the machine that has become American politics. Imagine what we could do if 10% or even 1% of the money our presidential candidates raised this year went to fund a program that directly benefited the American people instead of this very exhausting and negative theatrical production. This tracker shows the current tally at $3.08 billion. For what?
I was suddenly awake and paying very close attention to politics. I consumed news, followed a variety of public figures on Twitter and got connected with a diverse collection of the electorate on TikTok. And somewhere in that swirl, I realized: I would do anything in my power to make sure my daughter maintains control over her own reproductive decisions.
I’m honestly pretty terrified that I just admitted to the internet that I had an abortion. Not only did I have an abortion, I tried to have that same abortion multiple times.
That is a very simplified explanation of what it was and what I chose to do about it. Thanks to the courage of 33 public figures, I know I am not the only one. #HonestAbortion, #ShoutYourAbortion, #YouKnowMe
It shouldn’t matter that my life was at risk. I shouldn’t need an exception to make decisions about my own body. Sure, it might be mortal sin. But so is sex before marriage according to my devoutly Catholic grandmother. The Orthodox Rabbi in my family might also view eating a bacon cheeseburger as pretty unforgivable. The point is I’ve done both, so who knows what “sins” were already chalked up against me before I spent 12 weeks trying to save my own life by ending a pregnancy that could have killed me.
What kept me from sharing my story sooner was simple: I couldn’t control how people would react. The internet can be cruel. I didn’t want to open myself up to the rage, judgment, and sanctimony that swirl around this topic.
But the truth is this: I will never be able to control anyone’s reaction to a choice I’ve already made. So I shouldn’t let imagined reactions control whether I talk about it.
If you’re reading this and you feel compelled to respond, I hope you choose to respond like a human. If your faith is central to your identity, I’m happy for you. Truly. But please, don’t take what you believe and try to use it to control me. I think the best strategy to Make America Great Again is to just follow the concept of doing unto others what you would want done to you. Yosemite?
–––––––––––––––––––––––––––
In my professional life we have a process called “cause of error.” If a customer has a terrible experience, we dissect it: what happened, where it broke, how to fix it so no one else goes through the same thing.
So when I put that lens on my experience and substitute “pregnant woman” for “customer,” I arrive at the same conclusion: this was a systemic error that created a catastrophic human experience. And I hope that by telling this story, I can help prevent someone else from going through what I did.
There are two changes that can—and should—be made immediately:
#1: Produce relevant, medically accurate, and digestible information about cesarean scar ectopic pregnancies.
The information gap is enormous. That’s why I wrote ALL.THESE.WORDS.
It is still unclear how many women will ever face this diagnosis. But those who do deserve clear, accessible information about what it is, what the risks are, and what their options look like.
#2: Change the Methotrexate Multi-Dose Protocol
I recognize that my case was unusual. My doctor still hasn’t found another exactly like it and is working to publish it. I hope that case study helps inform future treatment. More importantly, I want the protocol changed so that once a patient enters Phase Two: Recovery, an ultrasound is required. It’s a simple safeguard that could confirm treatment success or catch failure early, potentially preventing months of unnecessary trauma.
–––––––––––––––––––––––––––
#1: Reach the undecided voter.
Reach even one undecided voter—or one who identifies as pro-life—and make them understand the stakes of this moment. Human rights are at risk. If this story resonates with you, share it. Or share your own. Whatever reaches the person who needs to hear it. This is how I honor Noah’s warrior spirit in this election. #BidenHarris2020
#2: Rename this diagnosis.
“Cesarean scar ectopic pregnancy” is a mouthful. Worse, the word “ectopic” causes confusion. It doesn’t convey the severity, the impossibility of the choices, or the risk to a mother’s life.
It was for this reason every time I spoke about it while telling this story, I used its full name. An acronym did not feel appropriate. If I had my way, I’d rename it “Noah’s Syndrome.”
–––––––––––––––––––––––––––
To summarize: the next presidential election concludes in four days. Whatever happens, we are at the beginning of an urgent battle to protect the constitutional right to control one’s own medical decisions. If you believe in that fight—even a little—consider donating your time, talent, or money to organizations working on the front lines:
- Access Reproductive Care – Southeast: helps women access reproductive care across Alabama, Florida, Georgia, Mississippi, South Carolina, and Tennessee.
- National Network of Abortion Funds: Raises funds to help eliminate economic barriers to abortion care.
- The Yellowhammer Fund: provides funding for abortion care as well as helping with other barriers to abortion like travel and lodging; based in Alabama.
- The oldies but goodies: Planned Parenthood, NARAL, ACLU
You could also consider becoming an abortion-clinic escort. Click here to learn more.
Phew. That was a lot. If you are still with me, thanks for making it to the end.
Stay well. Stay safe. Please vote.
@StevieNicks @LauraPrepon @Alyssa_Milano @Hannahgadsby @KekePalmer @aprilovegeary @linseygodfrey @ambertamblyn @Tess_Holliday @minkakelly @BusyPhilipps @jameelajamil @MillaJovovich @NICKIMINAJ @Joancollinsdbe @WhoopiGoldberg @chelseahandler @margaretcho @GloriaSteinem @MrsSOsbourne, @sherrieshepherd @BillieJeanKing, @jemimakirke, @VWOfficial, @LilKim, @NayaRivera, @rosemcgowan, @AshleyJudd, @RoArquette, @CynthiaNixon, @NelStamp, @KekePalmer, @RepSpeier
cc:
#control, #StopTheBans, #YouKnowMe, #HonestAbortion, #ShoutYourAbortion, #soonliving, #GrowingUpHerzog, #BidenHarris2020, #democracy, #NotoriousRBG, #WeDissent, #AwkwardFamilyPhotos, #PartyTime, #HandmaidsTale, #ScarlettLetter, #LifeGoals, #JamSession, #ER, @CDCgov, @LivingUrn, @JoeBiden, @ERANowAPI, @ARC_Southeast, @AbortionFunds, @YellowFund, @PPFA, @NARAL, @ACLU, @RBGmovie, @housetv, @onthebasisofsex, @MrsAm_FXonHulu, @nbcthegoodplace, @TheNewsroomHB0, @RuthSoukup, @AbbyRike, @NBCNewAmsterdam, @ResidentFOX, @NBCTransplant, @CodeBlackCBS, @HandmaidsOnHulu, @Ann_Dowd_, @alexisbledel, @samirawiley, @GreysABC, @katewalsh, @EllenPompeo, @PatrickDempsey, @HaylieGrammer, @SenGaryPeters, @mrsjfroco, @chrissyteigen, @johnlegend
Become An Official SooN LIVING Fan*
Learn how to tame YOUR chaos with exclusive content, productivity hacks and the occasional funny story.
*A low-risk time commitment; unsubscribe anytime.
Feedback? Input? Questions?
We cannot wait to hear from you!
10 Comments
Trackbacks/Pingbacks
- Growing Up Herzog - SooN LIVING - […] Put differently, it sucked. If you’re interested in the full drama — www.soonliving.com/control […]

Dear Elisha, Thank you for sharing your story with me, both in person at our visits and through this incredible essay in four acts. Your words brought me to tears many times, tears for you, your husband, your family including Noah, for our country, for women who will have the resources to navigate these painful waters and for those who won’t. The medical system is often not kind, nor compassionate, nor understandable, nor geared towards caring for the whole person/family. Yet within your story I’m relieved there were touchstones in the medical world who leaned in, touched your heart and guided you through. I hope I was one of those as well. I’m sorry for the pain you suffered and I thank you for your words and the activism you inspire. So needed in these crazy times.
Elisha – how incredibly strong you are to weather that time in your life, and to put pen to paper and share your story. It is because of strong people like you, others can learn and more fully understand your experience. Sending you lots of love and respect. Thank you for sharing, you are a role model of resilience. <3
Thank you so much for sharing your story, and all of this information that I sincerely hope other people in similar situations. This is incredibly brave and thoughtful.
You’re right – there’s so little information about this out there. I learned so much, and if it’s alright with you, if I know someone who is facing such a heartbreaking situation, I would like to share this article with them so they know what they might expect.
Elisha, Wow! What an incredible post. I am so sorry you went through this. Thank you for sharing your emotional journey and opening your self up to others. I know many people who can relate to your post. Such a lovely way to honor Noah. You had me in tears. Thank you for spreading awareness of Noah’s Syndrome.
Elisha,
I read every last word and am thankful you have courageously shared your very personal journey. Honest sharing paves the way for others to open up, share and connect with one another. I admire your truth and strength!
Xo
Elisha,
I am so sorry you had to go through something like this. I’m inspired and empowered by your story – I know it’s an important part of the healing process to tell it. Anti-abortion laws (amongst many, many other things) are an output of male oppression of women and making our voices heard is our best course of action. Almost 1 year ago I walked out of mass in Seattle and haven’t returned after the priest used shame as a teaching mechanism. I’ve never been as proud of that as I am today after reading your blog. I will spread the word on Noah’s Syndrome.
P.S. Jay’s comment above made me tear up – how luck you are.
Elisha- you are so courageous for sharing your story in such a unique time of our lives. Your ability to story-tell such a heart wrenching experience is truly remarkable. I know your story will make history and Noah will always be remembered and honored.
Thank you sharing xoxo
Elisha
I applaud your courage in coming forward with this story, because it has been such a long, mostly private emotional journey. It is also strewn with political landmines, which you’ve been (understandably) wanting to avoid. But your truth is so necessary at this time.
You and I experienced some of these tragic moments together. There are certainly some shared memories that bind us together in our sorrow, and longing for Noah to be with us today. Yet, I have still struggled to understand your innermost feelings. Your story, so well written, helped me walk a mile in your shoes. I would suspect you understand yourself a little better, too.
I am so proud to call you my life partner. You are a shining star that continues to burn brighter. I stand behind you always, as your biggest supporter to the end.
Your Husband,
-Jay
Such a raw and powerful retelling. Thank you for sharing this story and your healing journey. What a beautiful way to honor Noah. So much love for you, elisha.
Elisha, my Beautiful Princess.
I am so proud of how courageously, you faced your life!
I cried, all over again with your pain. Thank you for sharing and exposing yourself to HELP OTHERS. You are a LIGHT for many who thought they didn’t have any choices or HOPE to those who had to face the difficult ones. They can know they are NOT alone.
I’M SO PROUD of you. You’re one Class Act! Thank you for being my daughter. I will always love you. Mom